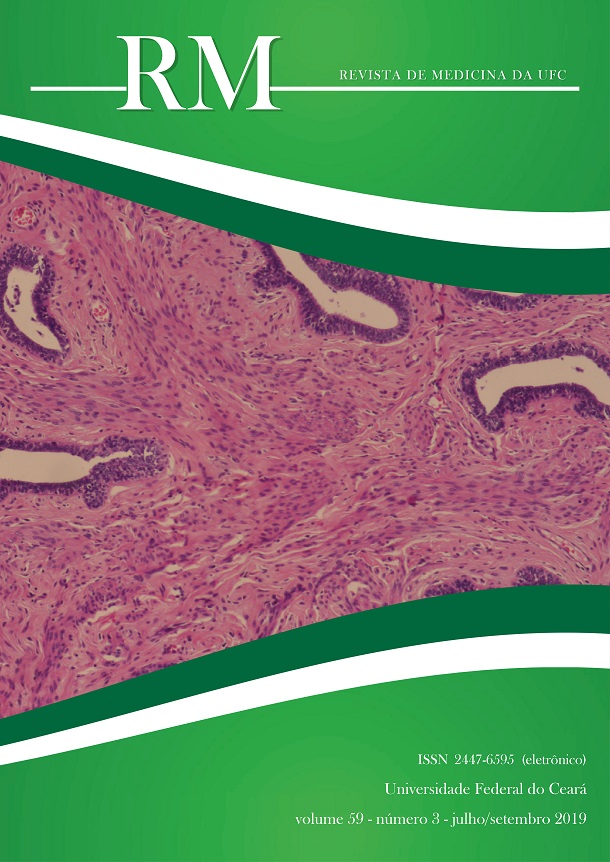
Rectal distention increases the frequency and duration of transient lower esophageal sphincter relaxations in anesthetized dogs– a putative rectoesophageal reflex
DOI:
https://doi.org/10.20513/2447-6595.2019v59n3p24-31Palavras-chave:
Esophago-gastric junction, Rectum, DogsResumo
Introduction: The esophagus is subject to frequent reflux of gastric contents as a normal phenomenon during episodes of transient lower esophageal sphincter relaxation (tLESR), responsible too, for pathologic reflux. However, pathologic reflux is mostly associated with reflux of acid contents. Distending the stomach provokes an increase in frequency of tLESR. Objective: To investigate the effect of distending the rectum on the tLESR and possible involved pathways. Methods: Forty four (Protocol: 096/07) street dogs were selected and divided into respective protocols: Rectal distention (RD), Gastric distention (GD), RD+GD, Atropine+RD, Hexamethonium+RD, Baclofen+RD, Bilateral Pudendal nerve section+RD and Spinal cord transection+RD. We determined and compared the tLESR of each group and subjected data to statistical analysis. Values of p<0.05 were regarded as statistically significant. Results: RD provoked a significant increase in the tLESR just as GD, with RD+GD provoking the highest value of tLESR. This increase in tLESR due to RD was prevented in A+RD, B+RD, Bilateral Pudendal nerve section+RD and Spinal cord transection+RD but not Hexamethonium+RD protocols. Conclusion: RD is a significant inducer of an increase in tLESR with participation of muscharinic and GABAβ, sensitive and spinal cord neurons, but not nicotinic receptors.
Referências
Martin CJ, Dodds WJ, Liem HH, Dantas RO, layman RD, Dent J. Diaphragmatic contribution to gastroesophageal competence and reflux in dogs. Am J Physiol. 1992; 263: G551-7.
Hershcovici T, Mashimo H, Fass R. The lower esophageal sphincter. Neurogastroenterol Motil. 2011; 23:819-830.
Zerbib F, Bruley des Varannes S, Scarpignato C, Leray V, D’Amato M, Roze´ C, and Galmiche JP. Endogenous cholecystokinin in postprandial lower esophageal sphincter function and fundic tone in humans. Am J Physiol Gastrointest Liver Physiol 275: G1266–G1273, 1998.Am J Physiol Gastrointest Liver Physiol 278:578-584, 2000.
Shafik A, El-Sibai O. Esophageal and gastric motile response to rectal distension with identification of a recto-esophagogastric reflex. Int J Surg Investig. 2000; 1: 373-9.
Whorwell PJ, Clouter C, Smith CL. Oesophageal motility in the irritable bowel syndrome. Br Med J (Clin Res Ed). 1981; 282:1101-2.
Coremans G, Geypens B, Vos R, Tack J, Margaritis V, Ghoos Y, et al. Influence of continuous isobaric rectal distension on gastric emptying and small bowel transit in young healthy women. Neurogastroenterol Motil 2004; 16: 107-111.
Youle MS, Read NW. Effect of painless rectal distention on gastrointestinal transil of solid meal. Dig Dis Sci 29: 902-906, 1984.
Palheta M S, Graça JRV, Santos AA, Lopes LH, Palheta R C, Souza MAN. The participation of the nitrergic pathway in increased rate of transitory relaxation of lower esophageal sphincter induced by rectal distension in dogs. Arq Gastroenterol, 2014 (2), 102–106.
Stephen AM, Haddad AC, Philipps SF. Passage of carbohydrate into the colon. Direct measurements in humans. Gastroenterology 1983; 85: 589–595.
Piche T, Zerbib F, Bruley des Varannes S, Cherbut C, Anini Y, Roze´C, Le Quellec A, Galmiche JP. Modulation by colonic fermentation of LES function in humans. Am J Physiol Gastrointest Liver Physiol 2000; 278: G578–G584.
Patrikios J, Martin CJ, Dent J. Relationship of transient lower esophageal sphincter relaxation to postprandial gastroesophageal reflux and belching in dogs. Gastroenterology 1986; 90: 545-51.
Murray JA, Clouse RE, Conklin JL. Components of the standard oesophageal manometry. Neurogastroenterology and Motility, (2003). 15(6), 591–606.
Lehmann A, Jensen JM, Boeckxstaens GE. GABAB receptor agonism as a novel therapeutic modality in the treatment of gastroesophageal reflux disease. 2010; 58: 287-313.
Jensen J, Lehmann A, Uvebrant A, Carlsson A, Jerndal G, Nilsson K, Frisby C, Blackshaw LA, Mattsson JP. Transient lower esophageal sphincter relaxations in dogs are inhibited by a metabotropic glutamate receptor 5 antagonist. Eur J Pharmacol. 2005 Sep 5;519(1-2):154-7.
Cox MR, Martin CJ, Dent J, Westmore M. Effect of general anesthesia on transient lower oesophageal sphincter relaxations in the dog. Aust NZ J Surg 1988; 58:825-830.
Sifrim D, Miau Y, Missotten T, Ni Y, Holloway R, Janssens J. Esophageal short¬ening and transient lower esophageal sphincter relaxations (TLESRs) in cats. Neurogastroenterol Motil. 1998; 10:98.
Franzi SJ, Martin CJ, Cox MR, and Dent J. Response of canine lower esophageal sphincter to gastric distension. Am J Physiol Gastrointest Liver Physiol 259: G380–G385, 1990.
Stakeberg J, Lehmann A. Influence of different intragastric stimuli on triggering of transient lower oesophageal sphincter relaxation in the dog. Neurogastroenterology and Motility (1999); 11(2), 125–132.
Holloway RH. The anti-reflux barrier and mechanisms of gastro-oesophageal reflux. Best Pract Res Clin Gastroenterol 2000; 14: 681-99.
Maggi CA, Manzini S, and Meli A. Contribution of neurogenic and myogenic factors in the response of rat proximal colon to distension. Am J Physiol Gastrointest Liver Physiol 252: G447– G457, 1987.
Jain NK, Boivin M, Zinsmeister AR, Brown ML, and Malagelada JR. Effect of ileal perfusion of carbohydrates and amylase inhibitor on gastrointestinal hormones and emptying. Gastroenterology 96: 377–387, 1989.
Layer P, Peschel S, Schlesinger T, and Goebell H. Human pancreatic secretion and intestinal motility: effects of ileal nutrient perfusion. Am J Physiol Gastrointest Liver Physiol 258: G196–G201, 1990.
Qi H, Brining D, Chen JD. Rectal distension inhibits postprandial small intestinal motor activity partially via the adrenergic pathway in dogs. Scandinavian Journal of Gastroenterology, 2007. Jul; 42 (7): 807-13
Nellgård P, Jönsson A, Bojö L, Tarnow P, Cassuto J. Small-bowel obstruction and the effects of lidocaine, atropine and hexamethonium on inflammation and fluid losses. Acta Anaesthesiologica Scandinavica. 1996. Mar; 40 (3): 287-92.
Salapatek, A. M. F., J. E. T. Fox-Threlkeld, and E. E. Daniel. Mechanism of nitric oxide(NO)-induced LES relaxation involves intracellular calcium modulation (Abstract). Gastroenterology 110: A750, 1996.
Mittal RK, Holloway R, Dent J. Effect of Atropine on the Frequency of Reflux and Transient Lower Esophageal Sphincter Relaxation in Normal Subjects. Gastroenterol 1995 Nov; 109(5):1547-54.
Farré R, Sifrim D. Regulation of basal tone, relaxation and contraction of the lower oesophageal sphincter. Relevance to drug discovery for oesophageal dis-orders. Br J Pharmacol. 2008; 153:858-69.
Downloads
Publicado
Edição
Seção
Licença
Indicação de avaliadores (revisores): caso desejado, os autores podem sugerir de 1 a 3 especialistas para a revisão do manuscrito. O(s) revisor(es) deve(m) preencher os seguintes requisitos:
- ter nível de Especialização, Mestrado ou Doutorado no tema do manuscrito;
- não possuir conflito de interesses com os autores;
- não possuir vínculo com o trabalho submetido;
- o revisor sugerido pode ser um membro do corpo editorial ou não (revisor ad hoc);
Declaração
Transferência de Direitos Autorais
O(s) autor(es) vem por meio desta declarar que o artigo intitulado “TÍTULO DO ARTIGO” enviado para apreciação da comissão
editorial da Revista de Medicina da UFC é um trabalho original, que não foi publicado ou está sendo considerado para publicação em outra revista, que seja no formato impresso ou no eletrônico.
O(s) autor(es) do manuscrito, acima citado, também declaram que:
-
Participaram suficientemente do trabalho para tornar pública sua responsabilidade pelo conteúdo.
-
O uso de qualquer marca registrada ou direito autoral dentro do manuscrito foi creditado a seu proprietário ou a permissão para usar o nome foi concedida, caso seja necessário.
-
A submissão do original enviada para a Revista de Medicina da UFC implica na transferência dos direitos de publicação impressa e digital.
A declaração original deve ser assinada, datada e encaminhada por e-mail: (revistademedicina@ufc.br).
Nota: Todas as pessoas relacionadas como autores devem assinar esta declaração. Não serão aceitas declarações assinadas por terceiros.